Cancer survival tied to protein levels
Researchers from KTH have used a big data medical study to identify genes that could help doctors predict a cancer patient’s prognosis.
Led by KTH Professor Mathias Uhlén , a team from the Science for Life Laboratory (SciLifeLab) hope to open a new path to personalized cancer treatment with today’s publication of the Human Pathology Atlas, which applies big data analysis to all genes in human cancer.
The release of the Human Pathology Atlas was accompanied by an August 18 article in Science , which reports that a large fraction of the human proteins is presented at different levels in cancers - and in many cases - have an impact on overall patient survival.
“These differences reinforce the need for personalized medicine in cancer treatment”, says Uhlén, who is Director of the Human Protein Atlas consortium and leader of the Human Pathology Atlas effort, as well as a Professor of Microbiology in the .
The Human Pathology Atlas was created as part of the Human Protein Atlas project to explore the role of cancer protein-coding genes in determining survival. Using metadata from 8,000 patients, as well as 2.5 petabytes of open source data, the researchers were able to generate gene expression models for individual patients, identifying key genes involved in tumor growth.
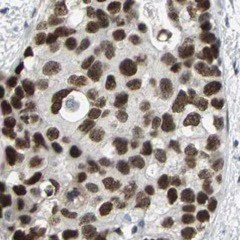
The researchers made a systems-based analysis of the transcriptome and corresponding proteins in 17 different types of cancer, including cancer of the lung, kidney, breast, pancreas and skin. The analysis, which resulted in 900,000 individual survival plots, required 200,000 core hours in supercomputing time.


The analysis identified candidate prognostic genes associated with clinical outcome for each tumor type. And while no single general prognostic gene could apply to all 17 forms of the disease that were examined, the researchers reported that shorter patient survival was associated with increased cell signaling activity, or up-regulation, among genes involved in cell growth. This pattern also involved down-regulation of genes involved in cellular differentiation.
“This study differs from earlier cancer investigations, since it is not focused on the mutations in cancers, but the downstream effects of such mutations across all protein-coding genes,” Uhlén says.
Uhlén says the study shows the power of big data mining to transform medical research. “It also highlights the advantage of open access policies in science in which researchers share data with each other to allow integration of huge amounts of data from different sources,” he says.
The work relies heavily on the supercomputing power available to the Human Protein Atlas consortium, through SciLifeLab . Adil Mardinolgu , a SciLifeLab fellow and KTH researcher who led the project’s systems biology effort, says these resources can help transform cancer treatment. “We are now in possession of incredibly powerful systems biology tools for medical research – allowing for the first time genome-wide analysis of individual patients with regard to the consequence of their expression profiles for clinical survival.”
The study was financed by the Knut and Alice Wallenberg Foundation .
David Callahan
You can access the Pathology Atlas via an interactive open-access database ( www.proteinatlas.org/pathology ).