New technology mimics the body and reduces the amount of animal testing
A multiple organ-on-chip platform developed by researchers at KTH and Harvard University could drastically accelerate drug testing. The technology provides accurate predictions of drug effects prior to clinical testing.
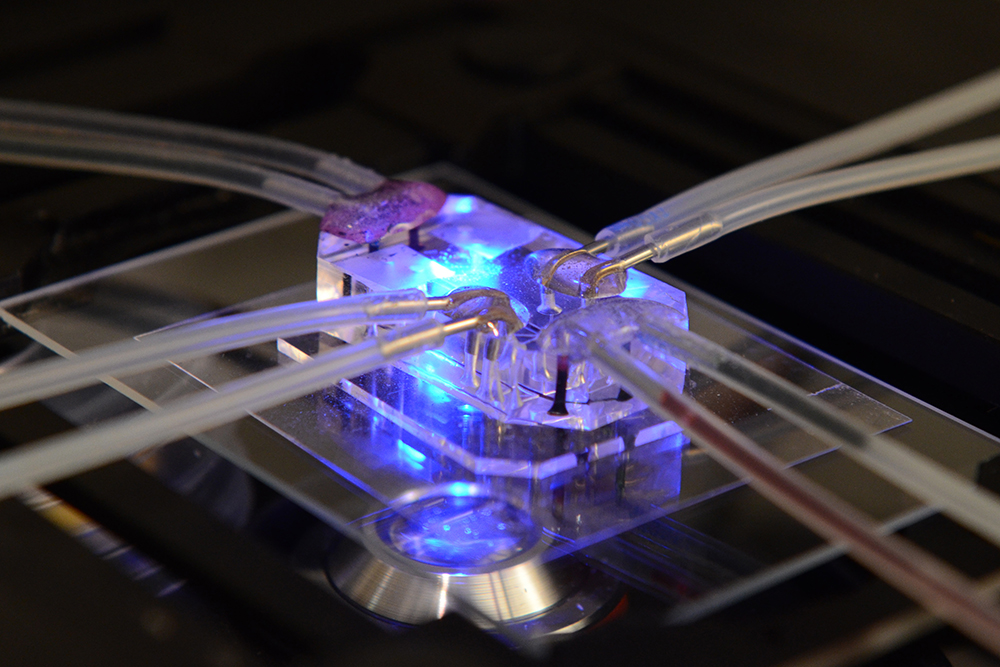
The body-on-a-chip device, which simulates eight organs of the human body, is enabled by an “interrogator” instrument that can culture up to 10 different organ chips, and sequentially transfer fluids between their endothelium-lined vascular channels to mimic normal human blood flow between the different organs of the body.
The advance was reported today in Nature Biomedical Engineering, in two articles (linked below) by lead author Anna Herland, a researcher in engineered in-vitro systems at KTH and the Wyss Institute for Biologically Inspired Engineering at Harvard. Funding of $37 million was provided by the U.S. Defense Advanced Research Projects Agency (DARPA).

Organ chips are microfluidic culture devices composed of a clear flexible polymer the size of a computer memory stick, which contains two parallel hollow channels that are separated by a porous membrane. Organ-specific cells are cultured on one side of the membrane in one channel, and vascular endothelial cells recapitulating a blood vessel line the other channel. Each channel is independently perfused with a cell type-specific medium. The porous membrane allows the two compartments to communicate with each other, and to exchange molecules like cytokines, growth factors and drugs, as well as drug breakdown products generated by organ-specific metabolic activities.
In order to predict changes in drug levels over time, as well as organ-specific toxicity, the team developed a computational scaling method to translate data – which is obtained from drug experiments involving three types of fluidically-linked organ chips – to the respective organ dimensions in the real human body. The approach enables for the first time accurate predictions of changes in drug levels over time – as well as organ-specific toxicities – that have been previously measured in human patients.
The technology aims to overcome major pain-points in the difficult and costly process of drug development. Failure rates in clinical trials that test new drugs for their safety and efficacy in humans remain high. According to current estimates, only 13.8 percent of all tested drugs demonstrate ultimate clinical success and obtain approval by the U.S. Food and Drug Administration (FDA). In addition to addressing these challenges, the new technology is expected to reduce the need for laboratory testing on animals.
One example where living animals must be used in preclinical testing is the characterization of a drug’s “pharmacokinetics” (PK), which involve the quantification of a drug’s absorption, distribution, metabolism and excretion (ADME). Together, these responses determine drug levels in the blood, and they involve interplay between many different organs linked by a vasculature containing flowing blood. Animals are also used to analyze drug “pharmacodynamics” (PD), or the effects that a drug produces on its target organs, which underlie its mechanism of action and its adverse effects.
The researchers studied the exchange of lifelike blood and drugs between individual organs, while also providing a way to carry out blood sampling that would mimic blood drawing from a peripheral vein. Among other steps, they looked at the pharmacological effects of cisplatin, a chemotherapeutic drug commonly used in cancer treatments, which is administered intravenously and displays unwanted toxicity in the kidney and bone marrow, Herland says.
The analysis closely reproduced the pharmacodynamic effects of cisplatin in patients, including a decrease in numbers of different blood cell types and an increase in markers of kidney injury, she says. “The in vitro-to-in vivo translation capabilities of the system produced quantitative information on how cisplatin is metabolized and cleared by the liver and kidney, which will make it possible for more refined predictions of drug absorption, distribution, metabolism, excretion and toxicity.”
David Callahan
Robotic fluidic coupling and interrogation of multiple vascularized organ chips